HEARING LOSS AND DEMENTIA
“I used to worry about my dad. I live out of state and call home weekly. On the phone, Dad didn’t seem like himself. He was aloof and sometimes unresponsive. I used to worry that he wasn’t following me on the phone or participating at family gatherings because of memory loss, dementia, or something else. But surely enough, once he could hear well, he was back to his old self. He smiled, laughed, and engaged in conversation just like he used to. Hearing aids were a game changer. They literally brought him back to life.”
During hearing aid consultations, family members often express concerns about hearing loss and the implications it can have on cognition and/or dementia. When individuals aren’t able to hear properly, they may seem disengaged, unresponsive, or they may respond inappropriately. Whether these changes in behavior result from hearing problems or reduced brain function is sometimes difficult to determine.
Hearing loss is one of the most common problems in the aging community. The prevalence of hearing loss increases with age, affecting 40% of people over 50 years old and roughly 71% of people over 70 years old. Untreated hearing loss can lead to difficulties when communicating and laxed participation in normal daily activities and social engagements. Withdrawal from these activities can ultimately lead to isolation, loneliness, and cognitive decline.
Hearing loss has been identified as potentially the most modifiable risk factor for dementia. One study found that age-related hearing loss is associated with an increased rate of cognitive decline and an increased risk of developing dementia. In addition, the likelihood for developing dementia increases with the severity of the hearing loss (Slade 2020).
WHERE DOES THE BREAKDOWN BEGIN?
So where exactly does hearing breakdown begin? The most common form of hearing loss seen in the aging community is formally known as “sensorineural” hearing loss. This hearing loss is either “sensory” or “neural” in nature. Sensory indicates that the hearing loss is caused by damage to the small sensory hair cells that are housed in the cochlea, the organ of hearing. The “neural” portion refers to the neurons that send the auditory message along the hearing nerve to the brain.
When the cochlea is not functioning properly, it is less effective at decoding and relaying signals to the hearing nerves. This compromised signal results in diminished neural activity. Both sensory and neural changes disrupt the brain’s ability to comprehend speech properly. This lack of input and change over time can alter how the brain allocates its resources. Think of the saying, “If you don’t use it, you’ll lose it!” I often explain to my patients that hearing is not just an “ear” thing, it’s an “ear-to-brain” connection!
THE EAR-TO-BRAIN CONNECTION
As we age, connections between brain cells can become lost or damaged. This disconnection is often referred to as cognitive decline. Research in hearing loss and cognitive decline has gained significant momentum over the past few years. Many studies continue to investigate the correlations and causal relationships between hearing loss and dementia. However, such study proves challenging since the brain and auditory systems are both quite complex. Even so, researchers have discovered evidence suggesting that changes are taking place at the level of the brain when hearing loss is present, particularly in the aging population (Slade et al. 2020).
Interestingly enough, research has demonstrated changes at the level of the brain in individuals with sensorineural hearing loss. One study that performed imaging on older adults to assess the brain’s activity while listening to sentences of varying speech rates found that individuals with sensorineural hearing loss experienced changes in brain activity while listening to faster talking rates than slower and simpler talking rates. Additionally, the study discovered reduced grey matter volume in the hearing portion of the brain–the portion responsible for processing information (Peele 2011)! Overall, people with hearing loss should focus on complex tasks because they are more profitable for the brain. In the real world, this equates to increased hearing effort, aka listening fatigue, when placed in those challenging listening environments. THINK: restaurant, large family gatherings, auditoriums, airports, etc.
Another study explored the association between hearing loss and dementia in the general population. They discovered that hearing loss is associated with significant increased risk of dementia, especially in patients aged 45 to 64 years. Their findings suggest that implementing early hearing protection, screenings, and hearing aids may help reduce this potential risk factor for dementia (Liu 2019).
WHAT CAN YOU DO?
So, what can you do to help yourself or your family members?
- Schedule a hearing test! It will NEVER hurt to have your hearing evaluated to establish a baseline. If we detect hearing loss, we can discuss options for moving forward.
- If you use hearing aids, wear them whenever you are awake. Keeping the brain stimulated, even in quiet situations, is important. The brain needs to hear all sounds to stay sharp and active–this includes the sink running, newspaper rustling, and feet stepping on the floor.
- Stay up to date on screenings and re-evaluate your hearing every one to two years. Hearing loss can happen gradually, and your brain might not know what it’s missing!
- If your family member struggles with dementia or Alzheimers, please know many hearing solutions can improve communication. Reach out to us. We can walk through various hearing technologies or accessories that will suit the needs of your loved one.
Since hearing loss is a modifiable age-associated condition linked to dementia, the Lancet International Commission on Dementia, Prevention, Intervention, and Care has estimated that treating hearing loss may decrease the risk of dementia by nine percent. The Hearing & Dizziness Clinic empowers patients and advocates that they treat hearing loss sooner rather than later!
During Alzheimer’s and Brain Awareness Month, we want to shed light on such a prevalent health topic. Experiencing Alzheimer’s, dementia, or any brain injury can be extremely challenging for our patients and their loved ones. At The Hearing & Dizziness Clinic, we have the patience, compassion, and empathy to walk through these challenges with you. Our goal is to ensure you and your loved ones are heard while helping you hear your best.
REFERENCES
Liu, Chin-Mei, and Charles Tzu-Chi Lee. “Association of hearing loss with dementia.” JAMA network open 2.7 (2019): e198112-e198112.
Peelle, Jonathan E., et al. “Hearing loss in older adults affects neural systems supporting speech comprehension.” Journal of neuroscience 31.35 (2011): 12638-12643.
Slade, Kate, Christopher J. Plack, and Helen E. Nuttall. “The Effects of Age-Related Hearing Loss on the Brain and Cognitive Function.” Trends in Neurosciences (2020).
Uchida, Yasue, et al. “Age-related hearing loss and cognitive decline—The potential mechanisms linking the two.” Auris Nasus Larynx 46.1 (2019): 1-9.

 Tinnitus Awareness Week is an important time to shed light on a condition that affects millions of people worldwide. If you or someone you love experiences a persistent ringing, buzzing, or hissing sound in their ears, you are not alone. Tinnitus can be frustrating, overwhelming, and, at times, life-altering. However, while there is no single cure for tinnitus, there are effective ways to manage it and significantly reduce its impact on daily life.
Tinnitus Awareness Week is an important time to shed light on a condition that affects millions of people worldwide. If you or someone you love experiences a persistent ringing, buzzing, or hissing sound in their ears, you are not alone. Tinnitus can be frustrating, overwhelming, and, at times, life-altering. However, while there is no single cure for tinnitus, there are effective ways to manage it and significantly reduce its impact on daily life.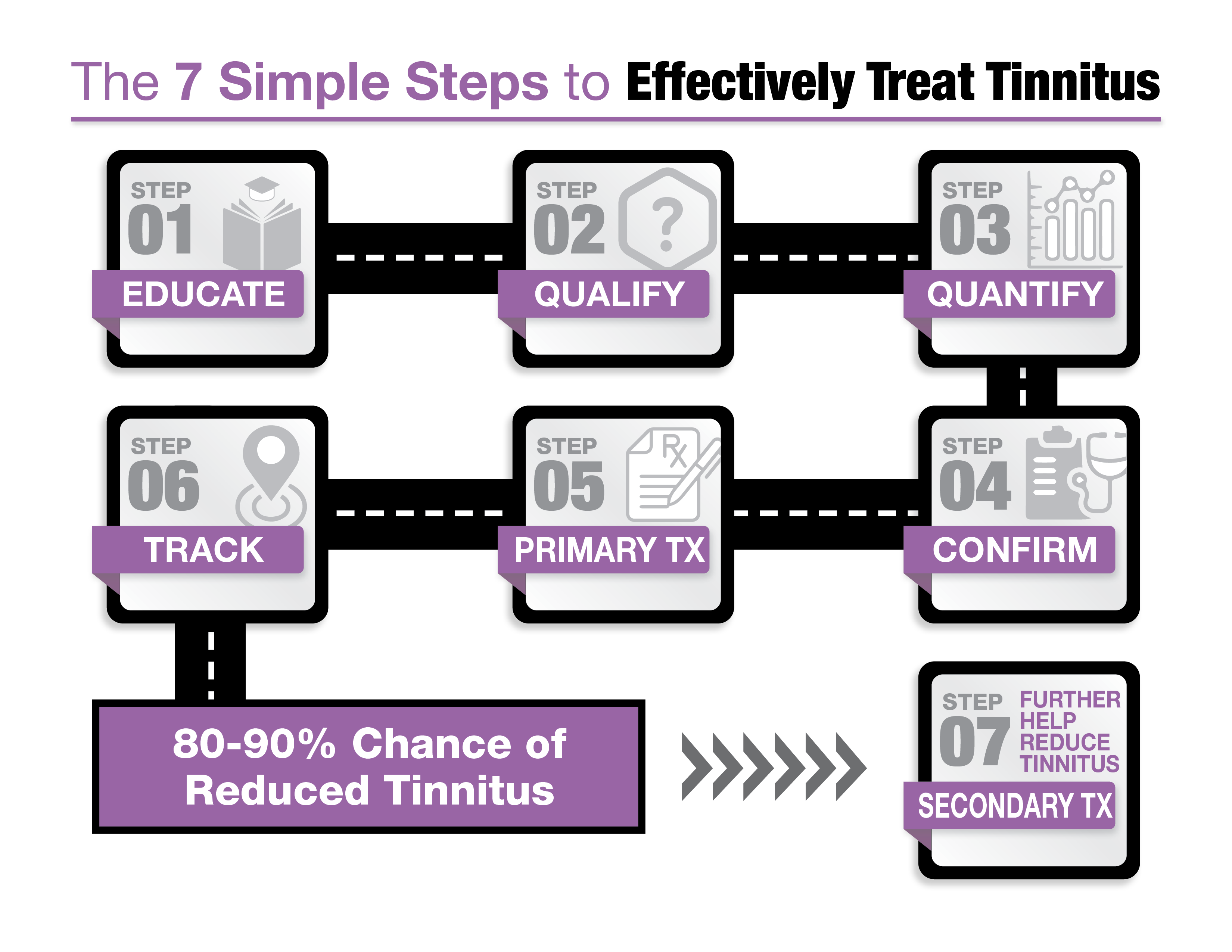 1. Education through Expert Resources
1. Education through Expert Resources I am Bernice McKenzie, an audiologist and the owner of The Hearing & Dizziness Clinic. Originally from Brantford, Ontario, I moved to Windsor to attend Wayne State University, where I was part of the first graduating class of Doctors of Audiology. Audiology, the study of hearing and balance disorders, provided me the opportunity to help people—a core value in my family of nurses and social workers. However, I soon realized that the profession was shifting towards hearing aid sales rather than patient care.
I am Bernice McKenzie, an audiologist and the owner of The Hearing & Dizziness Clinic. Originally from Brantford, Ontario, I moved to Windsor to attend Wayne State University, where I was part of the first graduating class of Doctors of Audiology. Audiology, the study of hearing and balance disorders, provided me the opportunity to help people—a core value in my family of nurses and social workers. However, I soon realized that the profession was shifting towards hearing aid sales rather than patient care.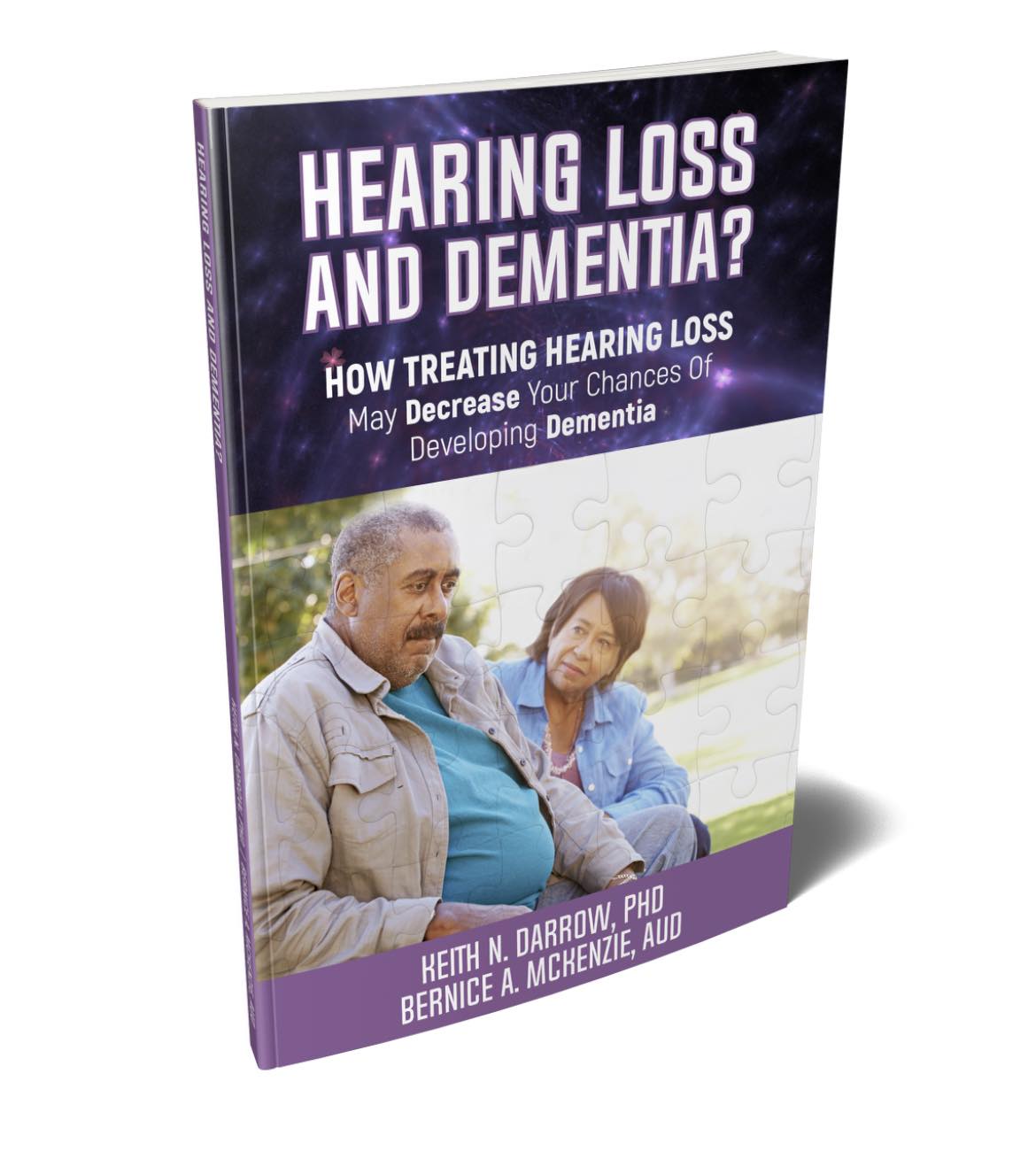 We understand that learning about tinnitus and hearing loss can feel overwhelming, which is why our new patient appointments last up to two hours. To help patients feel prepared and informed, we send them our pre-education book before their appointment. Co-authored by our owner, Bernice McKenzie, this book explains the treatment process in clear, easy-to-understand terms. It’s the perfect way to start your journey toward better hearing health.
We understand that learning about tinnitus and hearing loss can feel overwhelming, which is why our new patient appointments last up to two hours. To help patients feel prepared and informed, we send them our pre-education book before their appointment. Co-authored by our owner, Bernice McKenzie, this book explains the treatment process in clear, easy-to-understand terms. It’s the perfect way to start your journey toward better hearing health.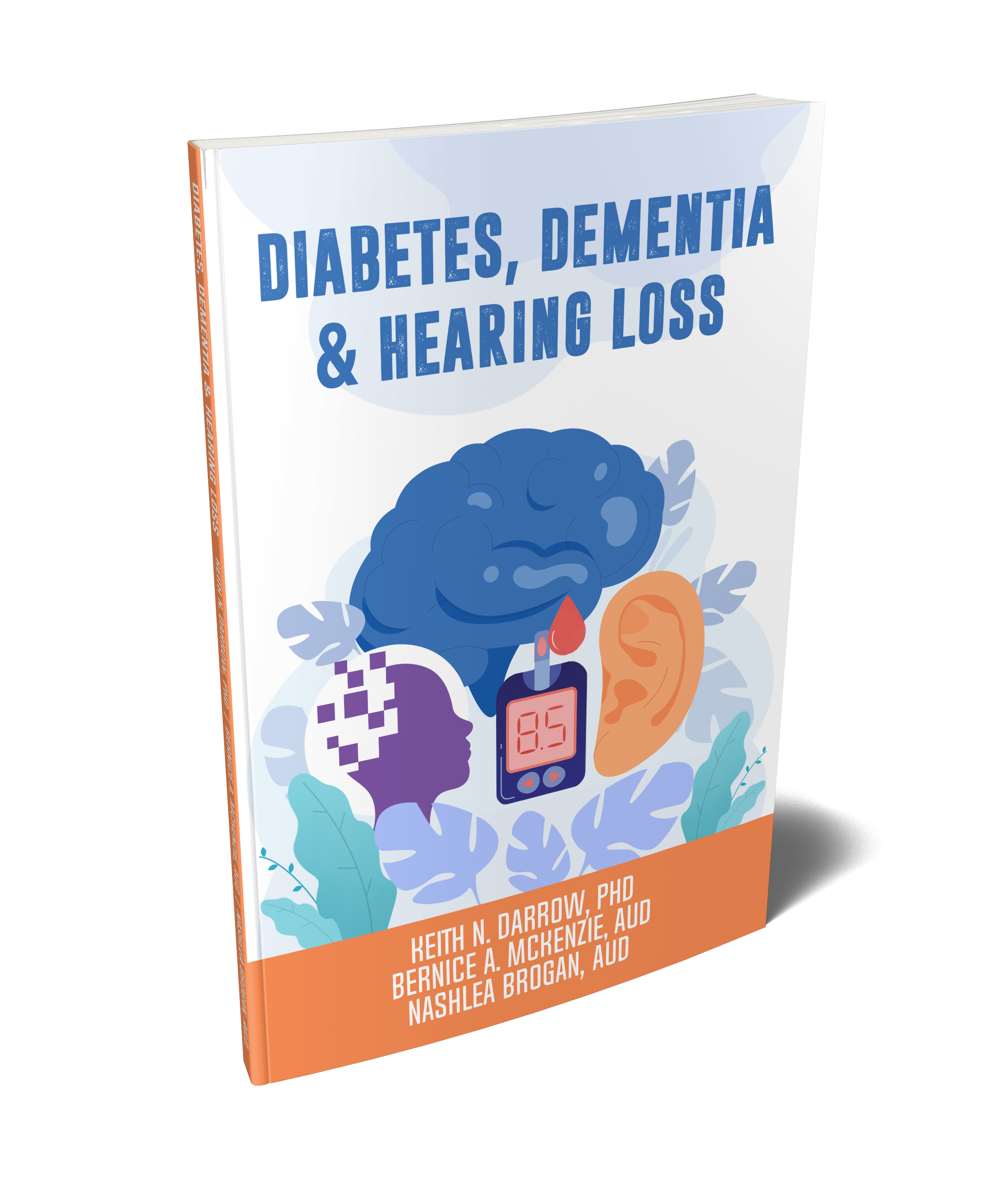 Did you know there’s a connection between diabetes, dementia, and hearing loss? This critical link inspired Bernice McKenzie to co-author a book on the topic. It’s an essential resource for anyone interested in understanding how these conditions interact and why treating hearing loss is so important for overall health. You can request your free copy by visiting
Did you know there’s a connection between diabetes, dementia, and hearing loss? This critical link inspired Bernice McKenzie to co-author a book on the topic. It’s an essential resource for anyone interested in understanding how these conditions interact and why treating hearing loss is so important for overall health. You can request your free copy by visiting  Tinnitus can be a frustrating and confusing condition, especially with so much conflicting information online. Dr. Keith Darrow’s book, “SILENCED. The Medical Treatment of Tinnitus”, is an excellent resource that cuts through the noise. It provides accurate, up-to-date information about tinnitus and treatment options in an easy-to-read format. This book is available free of charge—just request your copy today by clicking
Tinnitus can be a frustrating and confusing condition, especially with so much conflicting information online. Dr. Keith Darrow’s book, “SILENCED. The Medical Treatment of Tinnitus”, is an excellent resource that cuts through the noise. It provides accurate, up-to-date information about tinnitus and treatment options in an easy-to-read format. This book is available free of charge—just request your copy today by clicking  Retail locations often operate under the influence of hearing aid manufacturers, either directly or indirectly. Their primary goal is to sell as many hearing aids as possible. While hearing aids can undoubtedly be life-changing devices, it’s crucial to consider the impartiality of the recommendations provided in a retail setting. On the other hand, medical model clinics, like ours, are local and independently owned, with no affiliation to any specific hearing aid manufacturer. This allows us to prescribe the best solutions for our patients in an unbiased and personalized manner.
Retail locations often operate under the influence of hearing aid manufacturers, either directly or indirectly. Their primary goal is to sell as many hearing aids as possible. While hearing aids can undoubtedly be life-changing devices, it’s crucial to consider the impartiality of the recommendations provided in a retail setting. On the other hand, medical model clinics, like ours, are local and independently owned, with no affiliation to any specific hearing aid manufacturer. This allows us to prescribe the best solutions for our patients in an unbiased and personalized manner. We are always searching to add new services to our clinic. We’ve always offered wax removal, but now we offer what many are calling the “spa” version of ear wax removal. All three clinic locations now use the Earigator system to remove stubborn wax from your ears.
We are always searching to add new services to our clinic. We’ve always offered wax removal, but now we offer what many are calling the “spa” version of ear wax removal. All three clinic locations now use the Earigator system to remove stubborn wax from your ears. Affecting 1 in 8 people in North-America, hearing loss impacts almost every family with at least one person around the dinner table struggling to engage in conversations, missing the punchline of the joke and feeling isolated when they should be at their happiest. Whether the reason they haven’t treated their hearing loss is due to financial means or whether they’re refusing to accept that they may have some level of hearing loss, we are here as hearing healthcare providers to help.
Affecting 1 in 8 people in North-America, hearing loss impacts almost every family with at least one person around the dinner table struggling to engage in conversations, missing the punchline of the joke and feeling isolated when they should be at their happiest. Whether the reason they haven’t treated their hearing loss is due to financial means or whether they’re refusing to accept that they may have some level of hearing loss, we are here as hearing healthcare providers to help.