One sign of sudden sensorineural hearing loss could be the loss of at least 30dB of hearing in three connected frequencies within a 72 hour period.
Everyone’s hearing naturally declines with age, and people often have one ear that hears better than the other. If hearing loss appears suddenly in one ear for no apparent reason, you may have experienced a sudden sensorineural hearing loss, a kind of nerve deafness.
Those who experience sudden sensorineural hearing loss generally discover hearing loss when waking up in the morning. Others might notice when they try to use the deafened ear, such as using a phone. Many note a loud “POP” just before they lose their hearing. People with sudden deafness can also experience one or more of these symptoms: dizziness, feeling of ear fullness, ringing or buzzing in the ears (tinnitus).
If caught in time, sudden sensorineural hearing loss can be treated and corrected by an ear, nose and throat surgeon. Sudden sensorineural hearing loss symptoms should be seen as a medical emergency. Prompt treatment significantly increases the chance that at least some hearing can be recovered.
It is estimated that sudden sensorineural hearing loss affects between one and six people per 5,000 every year, but the actual number of new cases can be much higher, due to the fact that it often goes misdiagnosed. Sudden sensorineural hearing loss can affect people of all ages, but is most commonly seen in adults in their early 40s and 50s.
Diagnosing Sudden Sensorineural Hearing Loss
Ruling out conductive hearing loss, or hearing loss due to an obstruction such as fluid or wax in the ear is a good place to start. For sudden hearing loss without any clear cause upon examination, you should be referred to an ear, nose and throat surgeon and audiologist right away.
The ear, nose and throat surgeon can medically treat the condition at hand.
The audiologist will determine if the hearing loss is conductive or sensorineural with a diagnostic hearing test. Additional testing completed by the audiologist may include: (1) Tympanogram, (2) Acoustic reflexes, 3) Distortion product otoacoustic emissions (DPOAE) and/or (4) Auditory brainstem response (ABR). The information gathered by the audiologist will help guide the ear, nose and throat surgeons’ treatment plan.
What Causes Sudden Sensorineural Hearing Loss?
(1) Viral infections. One in four patients with sudden sensorineural hearing loss reports suffering from an upper respiratory infection within a month before the hearing loss. What virus causes sudden hearing loss? Viruses associated with sudden hearing loss include mumps, measles, rubella, as well as meningitis, syphilis and AIDS, among many others.
(2) Tumors. A variety of tumors in the ear, benign as well as malignant, may cause sudden sensorineural hearing loss.
(3) Head trauma affecting hair cells, eardrum or bones. Partial or total recovery from head injury induced hearing loss can be expected.
(4) Drugs and insecticides. Erectile dysfunction medications, a long list of prescription drugs and chronic abuse of painkillers may cause sudden hearing loss. Insecticides such as malathion and methoxychlor have been associated with sudden hearing loss in both ears (binaural sudden sensorineural hearing loss).
(5) Immunological disorders.
(6) Vascular disorders disrupting blood flow to the ear.
(7) Developmental abnormalities.
(8) Idiopathic disorders, such as multiple sclerosis, Meniere’s disease and others.
Sudden Sensorineural Hearing Loss Treatment
The most common treatment for sudden sensorineural hearing loss, especially when the cause is unknown, is corticosteroids administered by an ear, nose and throat surgeon. Steroids can treat many disorders and usually work by reducing inflammation, decreasing swelling, and helping the body fight illness. Additional treatments may be needed if you discover an underlying cause of your sudden sensorineural hearing loss.
It is very common for virally induced sudden hearing loss to be misdiagnosed as a middle ear infection. As a result, the typical treatments of middle ear infection, usually caused by bacteria, do not affect the virus actually causing the problem.
HOW DO YOU RECOGNIZE THE DIFFERENCE?
| SYMPTOM |
MIDDLE EAR INFECTION |
VIRAL EAR INFECTION |
| Hearing loss in both ears |
Frequently |
Rarely |
| Pain |
Frequently |
Never |
| Pressure in ears |
Frequently |
Sometimes |
| Dizziness, tinnitus or vertigo |
Rarely |
Frequently |
| Onset |
Gradual |
Sudden |
| Appearance of eardrum |
Fluid behind eardrum or
it looks opaque |
Appears normal |
| Drainage |
Sometimes |
Never |
| Usual treatments |
Antibiotics |
Trans-tympanic steroid injection |
| Misdiagnosis leads to |
Spread of infection to other parts of the head |
Permanent hearing loss |
 🚨 WINDSOR – GET READY! 🚨
🚨 WINDSOR – GET READY! 🚨
 Tinnitus Awareness Week is an important time to shed light on a condition that affects millions of people worldwide. If you or someone you love experiences a persistent ringing, buzzing, or hissing sound in their ears, you are not alone. Tinnitus can be frustrating, overwhelming, and, at times, life-altering. However, while there is no single cure for tinnitus, there are effective ways to manage it and significantly reduce its impact on daily life.
Tinnitus Awareness Week is an important time to shed light on a condition that affects millions of people worldwide. If you or someone you love experiences a persistent ringing, buzzing, or hissing sound in their ears, you are not alone. Tinnitus can be frustrating, overwhelming, and, at times, life-altering. However, while there is no single cure for tinnitus, there are effective ways to manage it and significantly reduce its impact on daily life.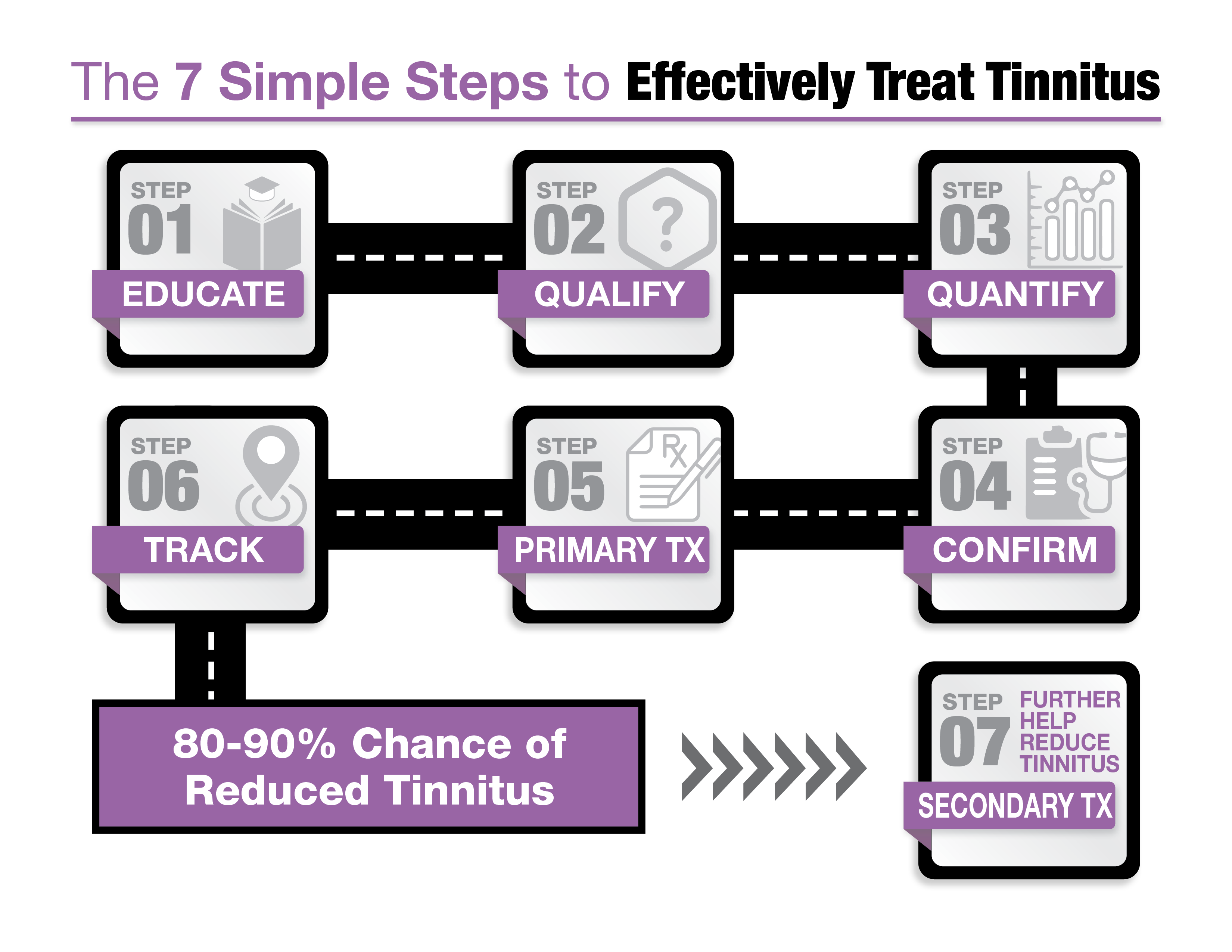 1. Education through Expert Resources
1. Education through Expert Resources I am Bernice McKenzie, an audiologist and the owner of The Hearing & Dizziness Clinic. Originally from Brantford, Ontario, I moved to Windsor to attend Wayne State University, where I was part of the first graduating class of Doctors of Audiology. Audiology, the study of hearing and balance disorders, provided me the opportunity to help people—a core value in my family of nurses and social workers. However, I soon realized that the profession was shifting towards hearing aid sales rather than patient care.
I am Bernice McKenzie, an audiologist and the owner of The Hearing & Dizziness Clinic. Originally from Brantford, Ontario, I moved to Windsor to attend Wayne State University, where I was part of the first graduating class of Doctors of Audiology. Audiology, the study of hearing and balance disorders, provided me the opportunity to help people—a core value in my family of nurses and social workers. However, I soon realized that the profession was shifting towards hearing aid sales rather than patient care. We understand that learning about tinnitus and hearing loss can feel overwhelming, which is why our new patient appointments last up to two hours. To help patients feel prepared and informed, we send them our pre-education book before their appointment. Co-authored by our owner, Bernice McKenzie, this book explains the treatment process in clear, easy-to-understand terms. It’s the perfect way to start your journey toward better hearing health.
We understand that learning about tinnitus and hearing loss can feel overwhelming, which is why our new patient appointments last up to two hours. To help patients feel prepared and informed, we send them our pre-education book before their appointment. Co-authored by our owner, Bernice McKenzie, this book explains the treatment process in clear, easy-to-understand terms. It’s the perfect way to start your journey toward better hearing health. Did you know there’s a connection between diabetes, dementia, and hearing loss? This critical link inspired Bernice McKenzie to co-author a book on the topic. It’s an essential resource for anyone interested in understanding how these conditions interact and why treating hearing loss is so important for overall health. You can request your free copy by visiting
Did you know there’s a connection between diabetes, dementia, and hearing loss? This critical link inspired Bernice McKenzie to co-author a book on the topic. It’s an essential resource for anyone interested in understanding how these conditions interact and why treating hearing loss is so important for overall health. You can request your free copy by visiting  Tinnitus can be a frustrating and confusing condition, especially with so much conflicting information online. Dr. Keith Darrow’s book, “SILENCED. The Medical Treatment of Tinnitus”, is an excellent resource that cuts through the noise. It provides accurate, up-to-date information about tinnitus and treatment options in an easy-to-read format. This book is available free of charge—just request your copy today by clicking
Tinnitus can be a frustrating and confusing condition, especially with so much conflicting information online. Dr. Keith Darrow’s book, “SILENCED. The Medical Treatment of Tinnitus”, is an excellent resource that cuts through the noise. It provides accurate, up-to-date information about tinnitus and treatment options in an easy-to-read format. This book is available free of charge—just request your copy today by clicking  We are honoured to present our distinguished speaker, Nashlea Brogan, Doctor of Audiology and Audiologist extraordinaire! With a passion for empowering those with hearing loss, Nashlea has dedicated her illustrious career to improving lives through the latest advancements and tools in Audiology.
We are honoured to present our distinguished speaker, Nashlea Brogan, Doctor of Audiology and Audiologist extraordinaire! With a passion for empowering those with hearing loss, Nashlea has dedicated her illustrious career to improving lives through the latest advancements and tools in Audiology. This educational event is designed to provide valuable insights into the correlations between diabetes, dementia, and hearing loss, and how they can impact your life. Don’t miss this opportunity to expand your knowledge and gain a deeper understanding of these crucial topics.
This educational event is designed to provide valuable insights into the correlations between diabetes, dementia, and hearing loss, and how they can impact your life. Don’t miss this opportunity to expand your knowledge and gain a deeper understanding of these crucial topics. Retail locations often operate under the influence of hearing aid manufacturers, either directly or indirectly. Their primary goal is to sell as many hearing aids as possible. While hearing aids can undoubtedly be life-changing devices, it’s crucial to consider the impartiality of the recommendations provided in a retail setting. On the other hand, medical model clinics, like ours, are local and independently owned, with no affiliation to any specific hearing aid manufacturer. This allows us to prescribe the best solutions for our patients in an unbiased and personalized manner.
Retail locations often operate under the influence of hearing aid manufacturers, either directly or indirectly. Their primary goal is to sell as many hearing aids as possible. While hearing aids can undoubtedly be life-changing devices, it’s crucial to consider the impartiality of the recommendations provided in a retail setting. On the other hand, medical model clinics, like ours, are local and independently owned, with no affiliation to any specific hearing aid manufacturer. This allows us to prescribe the best solutions for our patients in an unbiased and personalized manner. We are always searching to add new services to our clinic. We’ve always offered wax removal, but now we offer what many are calling the “spa” version of ear wax removal. All three clinic locations now use the Earigator system to remove stubborn wax from your ears.
We are always searching to add new services to our clinic. We’ve always offered wax removal, but now we offer what many are calling the “spa” version of ear wax removal. All three clinic locations now use the Earigator system to remove stubborn wax from your ears.